Orchiectomy for Transfeminine and Non-Binary Individuals
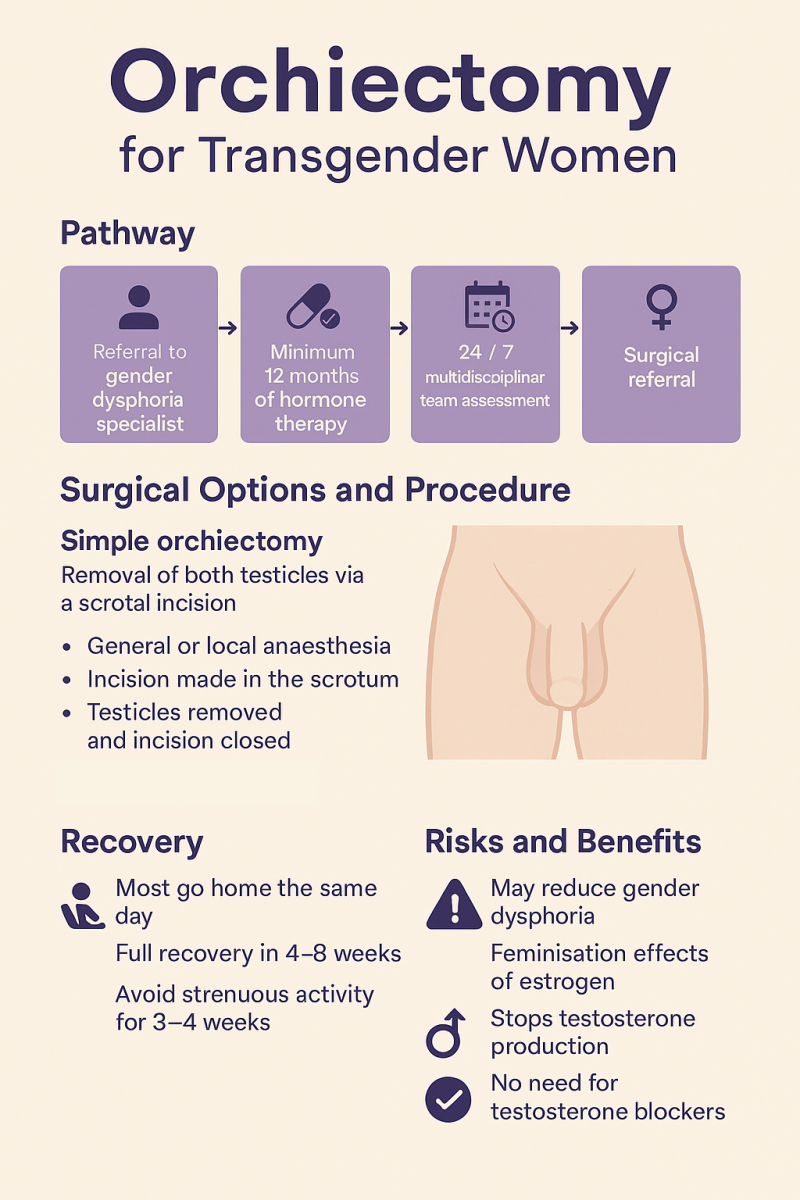
Orchiectomy, the surgical removal of one or both testicles, is a gender-affirming procedure that can be performed as a standalone intervention or as part of a broader transition plan. Under SOC8 (Standards of Care Version 8) from WPATH, orchiectomy is recognized as a medically necessary procedure for individuals experiencing persistent gender dysphoria related to their testes.

Surgical Process –
Surgical Options
- Simple Orchiectomy: Removal of both testicles via scrotal incision
- Radical Orchiectomy: Includes removal of spermatic cord (not typical for gender-affirming care)
- Scrotectomy (optional): Removal of scrotum; not recommended if planning vaginoplasty
Procedure Details
- Anaesthesia: General or local with sedation
- Incision made in the scrotum
- Testicles removed, blood vessels sealed
- Incision closed with dissolvable sutures
- Duration: 30–60 minutes
- Usually outpatient (same-day discharge)
Recovery Timeline
- Week 1–2: Rest, pain management, avoid heavy lifting and sex
- Week 3–6: Gradual return to normal activities
Full recovery: 4–8 weeks
Preparing for Your procedure Consultation with Mr Vahidi
During the Consultation
What to Expect:
- Meet Mr Vahidi who will take examine you and review your medical history.
- Sign consent forms and discuss photo documentation (optional).
- Discuss surgical options: simple orchiectomy vs. orchiectomy with scrotectomy (if applicable).
- Review risks, benefits, and recovery timeline.
Topics to Discuss
- What type of incision will be used?
- Will scrotectomy be performed? (Important if you’re considering future vaginoplasty)
- What is the expected recovery time?
- What post-op care will be provided?
- Will hormone therapy need to be adjusted after surgery?
Procedure Timeline
|
|

Time Off Work2-3 Weeks |

Hospital StayDay Case/Ovenight |

Bathing/Shower1 Week |

Walking1 Day |

Full Exercise4-6 Weeks progressive recovery and shoulder movement |

Compression GarmentsN/A |

Prone Sleeping1-2 Weeks |

Sexual Activity4-6 Weeks |

Full Recovery4-6 Weeks |

Driving4-6 Days |

Air Travel4 weeks |
Risks and Side Effects
- Short-term: Bleeding, infection, bruising, anaesthesia reaction
- Long-term: Infertility, fatigue, decreased libido, osteoporosis
- Psychological: Often positive impact on gender dysphoria
Benefits
- Stops testosterone production
- Reduces need for hormone blockers
- May improve feminisation effects of estrogen
- Reduces cancer risk
- Can simplify future vaginoplasty
- Often improves mental health and body confidence
Important Considerations
- Orchiectomy is irreversible
- Sperm banking recommended before surgery
- Lifelong hormone therapy required
- Discuss all options with your healthcare provider
Navigating Surgical Risks
Potential Complications of
Common Complications After
While procedure is generally a safe and has high satisfaction rates, like any surgical procedure, it carries some risks. These can vary depending on the surgical technique used
General Surgical Risks
- Bleeding: Excessive bleeding may occur during or after surgery
- Infection: Though rare, infections can develop at incision sites
- Poor wound healing: Delayed healing or wound reopening (dehiscence) may require medical attention
- Hematoma: A collection of blood under the skin that can cause swelling and pain
- Seroma: Fluid buildup under the skin, often managed with surgical drains
Procedure-Specific Risks
Anesthesia risks: Includes allergic reactions, airway issues, or heart complications